Example #1: Meet the Wonder Women of Indonesia
Rovina is one of hundreds of "wonder women" in Kopernik’s Wonder Women initiative that has empowered women to become clean energy micro-social-entrepreneurs, connecting life-changing solar lights, clean cookstoves, and water filters with last mile communities in some of Indonesia's poorest provinces.
More than 80 million people live without any electricity in Indonesia, and many more live with unreliable access to electricity.
Almost 100 million people rely on smoky, fuel-hungry three-stone fires for cooking.
And clean drinking water is often a costly luxury.
There is great demand for affordable, clean energy technologies, especially in the poorest provinces of eastern Indonesia, but geography and demography make energy access a huge challenge.
This is where Kopernik's Wonder Women Eastern Indonesia initiative comes in.
Equipping women with the skills and resources to become clean energy micro-social entrepreneurs is a viable, sustainable way of connecting these technologies with the people who need them the most.
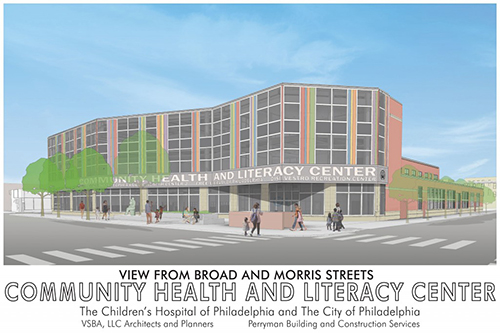
Example #2: Community Health And Literacy Center: A Health, Literacy & Recreation Hub
The Community Health and Literacy Center, formed out of a collaboration between the Children’s Hospital of Philadelphia (CHOP) and the City as unexpected partners, worked together to bring a neglected neighborhood both improved access to health care and health, promoting recreation and literacy opportunities.
The center, which opened in the spring of 2016, is a first-of-its-kind hospital-city partnership. The project includes a CHOP pediatric clinic; a full-service community health center run by the city’s department of public health; a branch of the Free Library of Philadelphia; and a modern recreation center with a playground and green space, run by the city’s Department of Parks and Recreation. It offers welcoming outdoor space for the neighborhood and an indoor community meeting space. The location has excellent public transit access, with a subway stop on site. CHOP and the city are working to integrate services and programming as a way to have more of an impact on improving population health.
Contributed by Lia Thompson, University of Kansas, Community Tool Box Intern.
Example #3: Vita Health & Wellness District: Health at the Center of a Neighborhood Transformation
The Vita Health & Wellness District project was established through a partnership between the Stamford housing authority and Stamford hospital to revitalize an impoverished inner city area, in Stamford Connecticut, into a mixed-income community with expanded neighborhood services centered around a sustainable urban farm. Addressing the social determinants of health provide a framework for managing the neighborhood transformation in ways that would support and strengthen the existing community.
The Vita project is a great example of how a hospital can fulfill the Affordable Care Act’s mandate to engage its community by partnering to address the social determinants of health. The project also demonstrates how a forward-thinking community development organization can effectively partner with the health sector to pursue comprehensive community revitalization that could not have been achieved otherwise. These are still early days in what promises to be a fruitful and long-lasting partnership.

Read more about the Vita Health & Wellness District project on the Building Healthy Places Network blog.
Contributed by Lia Thompson, University of Kansas, Community Tool Box Intern.
Example #4: Rolling Hills Apartments: Weaving Together Opportunities for Healthier Lives for a Diverse Immigrant Community

Twin Cities LISC, a local community development financial institution, has partnered with local organizations and city agencies to create quality affordable housing with improved healthcare access, including constructing a Federally Qualified Health Center. LISC also employed community health advocates to weave together the isolated health-related efforts in the neighborhood of focus into a cohesive health agenda. More specifically, they connect and help support existing efforts, identify and help address gaps, and facilitate the conversations and activities that sustain collaboration.
Learn how social determinants of health are being addressed to build healthier lives for immigrants in St. Paul, Minnesota in this Community Close-Up from the Building Healthy Places Network.
Contributed by Lia Thompson, University of Kansas, Community Tool Box Intern.
Example #5: Revitalizing People and Place with a Healthy Food Hub Origin

Following the devastation of Hurricane Katrina in New Orleans, the founders of what became Broad Community Connections (BCC) began to attend community meetings, and investigate with their fellow community members how to rebuild a city in disarray. These discussions highlighted many of the problems that many central New Orleans resident had faced even before the storm, including but not limited to economic disadvantage, community disinvestment, health disparities, and lack of access to many needed goods and services. BCC was designed to revitalize Broad Street, a commercial thoroughfare running through the heart of the city and to connect several of the central city neighborhoods.
Founded in 2008, BCC set its sights on improving health and improving economic vitality in the area. Ultimately, the ReFresh project provided a high-quality grocery store to a low-income food desert and created a multi-faceted hub to improve healthy food access and local food systems, foster community connectivity, support youth development, and anchor economic development.
Read more about the ReFresh project in New Orleans on the Building Healthy Places Network blog.
Contributed by Lia Thompson, University of Kansas, Community Tool Box Intern.
Example #6: Under One Roof: Health Care and Social Services in the Same Place
The Chicanos Por La Causa (CPLC) is the largest community development corporation based in Arizona. CPLC is committed to building stronger, healthier communities as a lead advocate, coalition builder, and direct service provider. CPLC helps more than 200,000 people through programs in four areas–housing, economic development, education, and health and human services. CPLC recognizes that the needs of the families it serves are complex as a family rarely approaches the CDC with only one need. As a result, CPLC sought to establish cross-sector partnerships that would more effectively and holistically meet the needs of families.
Read more about CPLC on Rooflines - The Shelterforce Blog, from the National Housing Institute.
Contributed by Lia Thompson, University of Kansas, Community Tool Box Intern.
Example #7: Boston Children’s Hospital Community Asthma Initiative
The Community Asthma Initiative (CAI), an initiative of Boston Children’s Hospital, began addressing health disparities in Boston neighborhoods impacted by asthma in 2005. CAI provides an enhanced model of care, which includes asthma education and home visits for families with children ages 2–18 living in the Greater Boston area that were previously treated in the Emergency Department (ED) or hospitalized as a result of asthma. CAI works with partners and coalitions to address asthma health disparities by implementing changes in policies at the local and state levels. As of June 2014 there were reductions in the number of children with ED visits, hospitalizations, missed school days, and missed work days for parents.
Read more about the Community Asthma Initiative from the National Forum on Hospitals, Health Systems & Population Health.
Contributed by Lia Thompson, University of Kansas, Community Tool Box Intern.
Example #8: It’s Not Just About the Buildings: How Community Development Organizations are Promoting Residents’ Mental Health
Around the country, housing and community development groups are increasingly stepping up to partner with residents to improve community well-being by proactively strengthening residents’ emotional and mental health. Read more.
Example #9: Pilot Project Directs Healthcare Resources to Rural Missouri

A pilot project has been announced that plans to improve health outcomes in rural Missouri communities. It’s a collaborative effort between the Missouri Department of Social Services and the MO HealthNet Division.
The Transformation of Rural Community Health (ToRCH) project focuses on addressing social care challenges that impact residents’ ability to maintain their health and manage chronic conditions.
“(It’s) a groundbreaking initiative that empowers and encourages rural communities to collaborate to address healthcare-related social needs among their Medicaid population, with a focus on driving better health outcomes,” said Robert Knodell, Missouri Department of Social Services Director.
One key focus of the project is to tackle social determinants of health that influence overall wellbeing – safe housing, transportation, access to healthy foods, and physical activity opportunities. The U.S. Department of Health and Human Services explained that these needs influence the conditions where people are born, grow, learn, work, play, worship, and age.
“For too long, our payment systems have failed to reward hospitals for efforts to address some of the root causes of poor health,” said Kirk Mathews, MHD Chief Transformation Officer, “The ToRCH program allows hospitals to receive payment for proactively addressing issues that contribute to poor health outcomes. Under this model, hospitals are empowered to truly be in the ‘healthcare’ business in addition to the ‘sick care’ business.”
Six rural hospitals were selected last June as part of the pilot project, in Salem, Clinton, Sedalia, Rolla, Bolivar, and Richmond. The funding allows them to act as community hubs.
Click here to read the full article at the MissouriNet website.